Clinicians and researchers from the New York University (NYU) Grossman School of Medicine, in collaboration with the APBD Research Foundation (APBDRF), have published an exciting paper in the Journal of the Neurological Sciences. The study introduces the first disease-specific patient-reported outcome (PRO) measure for APBD, offering valuable insights into this rare neurogenetic disorder. A team from NYU, including Genevieve Wilson, Dr. Xiaochun Li, Dr. Judith Goldberg, Dr. Heather Lau, and Dr. Nicolas Abreu developed this novel tool in collaboration with board members from APBDRF, Dr. Deberah Goldman and Harriet Saxe.
Currently, there are no disease-modifying therapies for APBD, so the development of the APBD questionnaire on Symptom burden and health-related Quality of life (APBD-SQ) represents a significant advancement in the ability to capture the patient and caregiver experience. This tool may have uses in the clinic to monitor APBD and also in clinical trials to determine treatment responsiveness.
Although existing PRO measures have been developed and validated for other conditions, they fail to capture the unique complexities of APBD. To address this gap, the lead authors of the study collaborated with patients, caregivers, clinicians, and the APBD Research Foundation to develop the APBD-SQ. This development process included a series of drafts, reviews, revisions, and pilot testing. Designed to be completed in about 15 minutes, the survey allows for proxy completion by caregivers. It includes a 23-item disease severity assessment addressing symptoms and a 22-item quality of life assessment, focusing on daily tasks such as getting in and out of bed or participating in social activities. A six-point scale was used to quantify the patient experience.
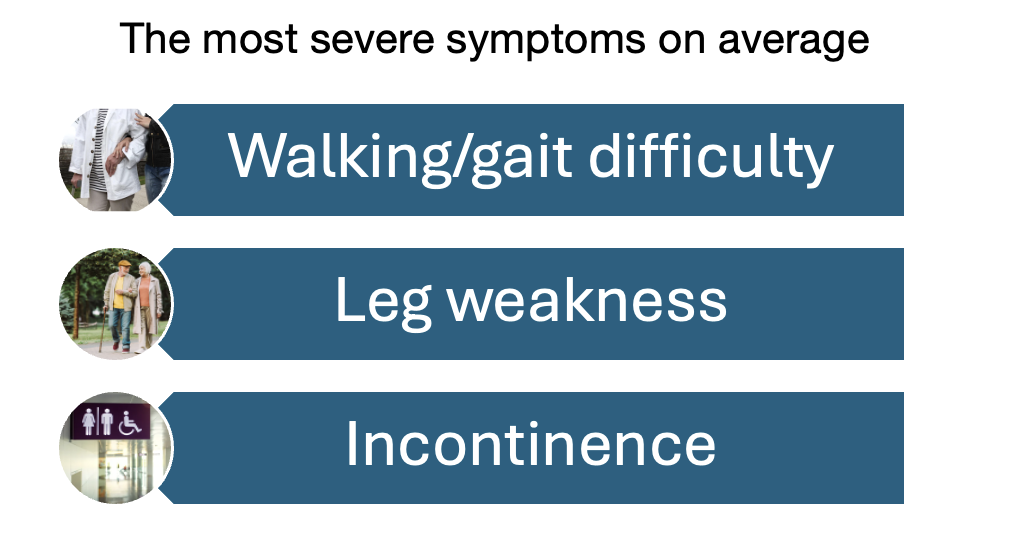
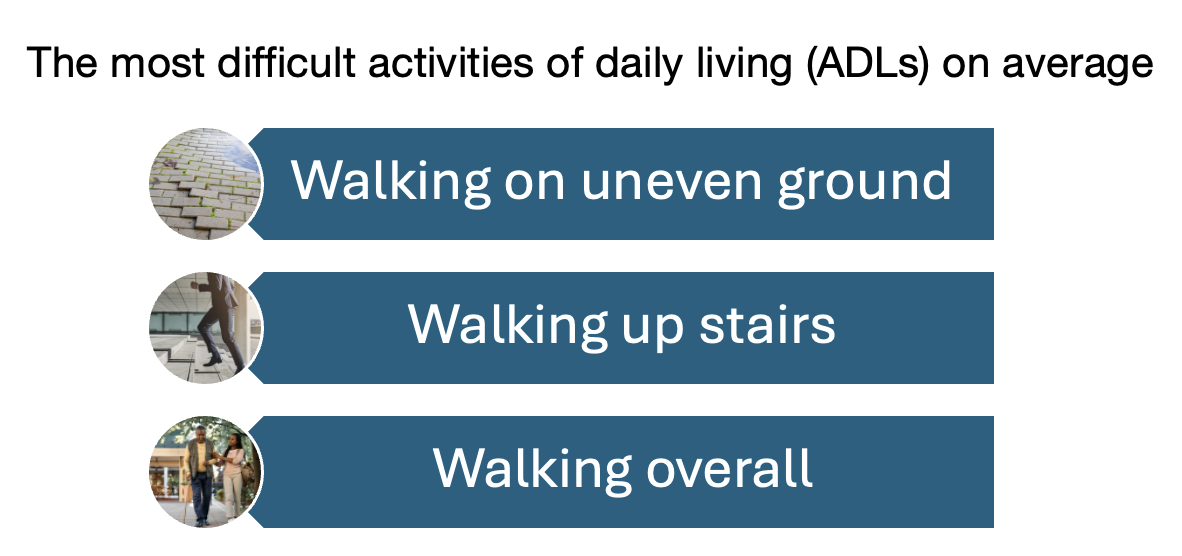
The study utilized an anonymous survey administered to patients having self-reported APBD diagnoses. Among the participants, 29 completed disease severity assessments, and 34 completed quality of life assessments. Most respondents were over 60, Ashkenazi Jewish, and not employed. The findings were consistent with existing literature, indicating that the onset of APBD can be expected by the 5th or 6th decade of life, with initial symptoms of bladder dysfunction followed by gait difficulties. The most severe symptoms reported were walking/gait difficulties, leg weakness, and incontinence, with the most challenging activities of daily living being walking on uneven ground, climbing stairs, and general mobility. Cluster analysis revealed naturally occurring groupings of certain symptoms, supporting internal validity of the questionnaire. Composite disease severity scores and composite health-related quality of life scores were calculated, identifying that higher scores had a statistically significant association with key aspects of day-to-day function, including unemployment and use of an assistive device. Older individuals were also noted to have higher composite quality of life scores, consistent with APBD’s progressive nature.
Overall, the findings suggest that this questionnaire may be a valuable tool for tracking disease progression in clinical settings and future clinical trials. The authors emphasize that these composite scores are particularly advantageous for capturing the lived experience of APBD across a broad range of functions in a single measure. However, the study’s cross-sectional design, inclusion of the caregiver perspective, and small sample size should be recognized as potential limitations. Future research should aim to validate this questionnaire in a larger, more diverse population over time.
Editor’s Note: “Research Highlights” is an ongoing feature in our newsletter. It is focused on scientific publications of interest to our community. Our thanks to researchers at NYU Grossman School of Medicine for sharing their research with us in the August 2024 edition of our e-newsletter!
